Medicare and Medicaid: Additional Actions Needed to Enhance Program Integrity and Save Billions
Fast Facts
Both Medicare and Medicaid are susceptible to payment errors—over $100 billion worth in 2023. Known as "improper payments," these are payments that are either made in an incorrect amount or should not have been made at all.
We testified about our numerous recommendations to CMS and Congress that reduced improper payments, enhanced program integrity, and saved billions of dollars in Medicare and Medicaid.
Other recommendations remain unimplemented. For example, we recommended that Congress take action to address that Medicare pays more for certain services based on where they are provided. Doing so could save Medicare $141 billion over 10 years.

Highlights
What GAO Found
The Department of Health and Human Services (HHS) estimated a combined total of over $100 billion in improper payments in the Medicare and Medicaid programs in fiscal year 2023. This represents 43 percent of the government-wide total of estimated improper payments that agencies reported for that year.
Improper Payments Estimates for Fiscal Year 2023
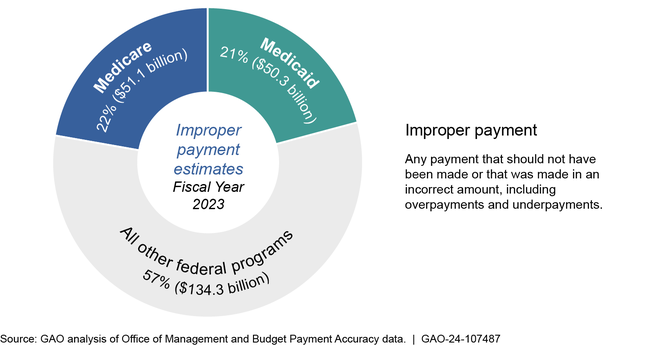
Note: Estimates also include payments whose propriety cannot be determined due to lacking or insufficient documentation.
The Centers for Medicare & Medicaid Services (CMS), within HHS, has taken several steps in response to GAO recommendations to help reduce improper payments in Medicare and Medicaid. These actions have resulted in billions of dollars in federal savings. For example:
- Improved fraud prevention in Medicare. CMS implemented capabilities that automatically stopped payments of certain improper and non-payable claims. These improvements generated an estimated almost $2 billion in savings over a 5-year period.
- Improved Medicaid managed care oversight. CMS worked with states and audit contractors to improve oversight. This included an exponential increase in investigations of managed care providers, from 16 in 2016 through 2018 to 893 in 2019 through 2021. Preliminary results indicate that the audits are identifying overpayments.
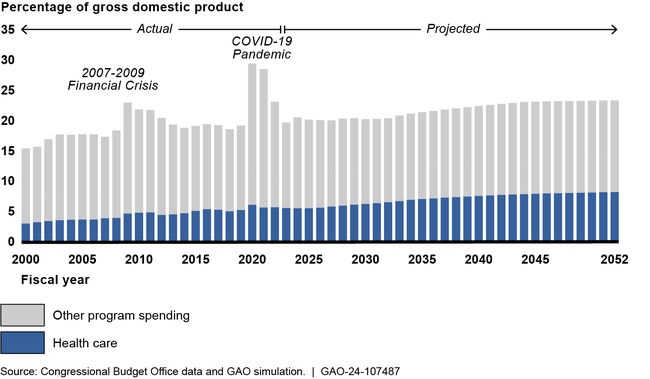
In the current fiscal environment, addressing improper payments and providing sufficient oversight of program spending, more generally, is particularly important. Federal spending for Medicare and Medicaid has grown by almost 80 percent over the past decade and growth in these and other health programs is projected to continue.
Health Care and Other Government Program Spending, Actual and Projected
CMS and congressional action on GAO recommendations related to Medicare and Medicaid has resulted in over $200 billion in financial benefits since 2006. Action on recommendations that remain unimplemented would further enhance program integrity and save billions of dollars in Medicare and Medicaid spending.
- Provider screening and enrollment. GAO recommended CMS expand its review of states' implementation of provider screening and enrollment requirements in Medicaid, and monitor progress when states are not fully compliant. For Medicare, GAO recommended that CMS implement a risk-based plan for revalidating enrollment for Medicare providers after pauses during the COVID-19 pandemic.
- Prepayment claim reviews in Medicare. GAO recommended that CMS seek legislative authority to allow Recovery Auditors to conduct prepayment claim reviews, which are generally more cost effective than postpayment reviews in preventing improper payments.
- Equalizing certain Medicare payments. GAO recommended that Congress take action to address that Medicare pays more for certain services based on where they are provided. Congress has taken some actions. For example, this committee proposed and the House passed legislation to equalize payments for certain drug administration services. Taking additional steps to equalize payments has been estimated to save Medicare $141 billion over 10 years.
- Telehealth. In response to the COVID-19 pandemic, HHS temporarily waived certain Medicare restrictions on telehealth and use increased dramatically. We recommended CMS comprehensively assess the quality of telehealth services in Medicare, which is needed to ensure those services are medically necessary, among other things.
- Medicaid demonstrations. In response to GAO recommendations, CMS has made changes to its policies for ensuring that demonstrations do not increase federal spending, reducing federal liabilities by over $120 billion. Additional action by CMS and Congress could result in further savings.
- State auditors. State auditors play an important role in Medicaid oversight and have identified improper payments and other deficiencies through their reviews. GAO recommended that CMS use trends in state auditor findings to inform its Medicaid oversight and share information on the status of actions to address findings with state auditors.
Why GAO Did This Study
In 2023, the Medicare program spent an estimated $1.0 trillion to provide health care services for approximately 66 million elderly and disabled individuals. This involved processing over a billion transactions. Medicaid is a joint federal-state program that finances health care for low-income and medically needy individuals. It is the second largest health care program by expenditures, with an estimated $849 billion in federal and state spending for services provided to about 90 million individuals in 2023.
Medicare and Medicaid are complex and large programs. They represented 26 percent of federal program spending in fiscal year 2023. The programs are susceptible to improper payments, as well as potential mismanagement and fraud, waste, and abuse. As a result, GAO added Medicare to its High-Risk list in 1990 and Medicaid in 2003.
This testimony focuses on examples of steps taken by CMS to reduce improper payments in Medicare and Medicaid, as well as actions still needed by CMS and Congress. It draws on GAO's reports issued and recommendations made from 2008 through 2024 on the Medicare and Medicaid programs and known steps CMS has taken to address these recommendations as of March 2024.
Recommendations
CMS has implemented dozens of GAO recommendations to improve Medicare and Medicaid. As of March 2024, over 100 recommendations to CMS remain unimplemented, including 15 related to improper payments.
