Science & Tech Spotlight: At-Home Tools to Diagnose Alzheimer's, Parkinson's, and Related Diseases
Fast Facts
Neurodegenerative diseases affect about 7 million people in the U.S., with cases expected to increase.
This Spotlight covers cognitive assessment apps and wearable sensors designed for home use. They can collect data on patients' cognitive and motor abilities and help detect symptoms of Alzheimer's and other neurodegenerative diseases.
Doctors can use data from these tools to diagnose diseases earlier and more accurately, and these tools can reduce the number of clinic visits for patients. But, some patients may not have access to smartphones or other technology required to use them, and apps that collect health data raise privacy concerns.

Highlights
Why This Matters
Neurodegenerative diseases such as Alzheimer’s and Parkinson’s can make day-to-day tasks challenging because they may affect cognitive, motor, and social function. Neurodegenerative diseases affect about 7 million people in the U.S. Researchers expect cases to increase as the population ages. Earlier detection of these diseases may help health care providers treat patients before the onset of severe symptoms and slow disease progression.
Key Takeaways
- At-home tools may facilitate earlier detection of neurodegenerative diseases.
- These tools can be a cost-effective way to collect information that is difficult to gather in a clinical setting.
- Health care providers can use information from at-home tools to help diagnose neurodegenerative disease, but such tools are not a replacement for clinical care.
The Technology
What is it? At-home tools collect and analyze patient data on certain indicators that relate to cognitive ability—memory, reasoning, and language—and motor function. This includes walking, writing, stability, and the presence of tremors. Tools such as digital cognitive assessments and wearable sensors have the potential to help health care providers detect and diagnose neurodegenerative diseases earlier and more accurately. The tools help assess patients in an environment more reflective of daily life, detect indicators that are challenging to observe in a clinical setting, and collect data on patients’ health over time. Traditional diagnostic approaches—which occur in a clinical setting such as a physician’s office—can be more invasive, less convenient, and may not identify these symptoms until the disease is more advanced.
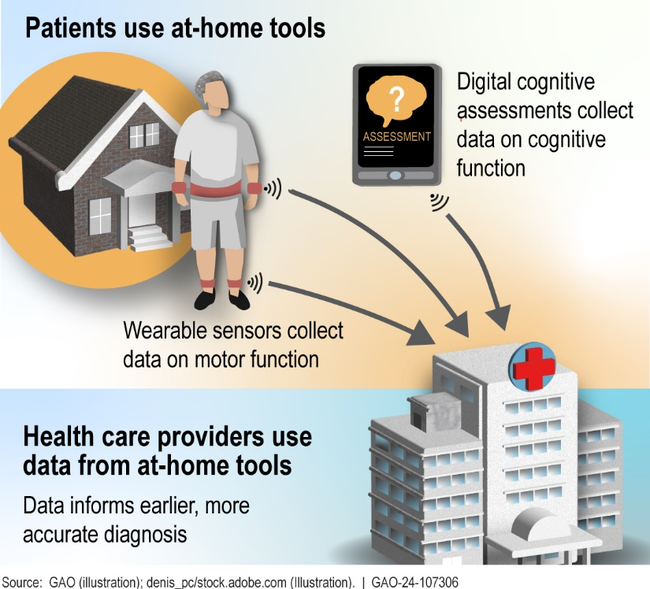
Figure 1: Patient and health care provider use of at-home tools
How does it work? Digital cognitive assessments use web- or application-based technologies to gather data on a patient’s cognitive abilities. For example, one activity asks patients to memorize objects and their position in a pictured room.
Wearable sensors worn on or near the body measure a range of indicators. Sensors on the hands, wrists, or ankles can collect data on the speed and direction of movements—such as hand tremors, sway, or postural adjustments—that may be indicative of neurodegenerative disease. Smartphones equipped with movement sensors can collect similar data when worn near the body. Researchers found that smartphone sensors can identify whether a person exhibits symptoms associated with Parkinson’s disease based on the way they move.
How mature is it? Multiple manufacturers of digital cognitive assessments—which could be administered at-home—have registered with the Food and Drug Administration. However, such at-home assessments are not widely commercially available, and more research is needed on their accuracy.
Wearable sensors vary in their maturity and use. Specifically, sensors worn on the body are an established tool to assess mobility. Researchers call for further studies to investigate the accuracy of smartphone-based sensors prior to applying them more broadly in diagnosis.
Opportunities
- Provide data to support early diagnosis. Providers can use data from at-home tools to inform earlier or more appropriate interventions to slow cognitive decline and improve symptom management. As technologies mature, patients could also potentially use insights from at-home tools to decide whether they need to consult a provider.
- Reduce time and cost. At-home tools can be a practical and cost-effective way to reduce the number of clinic visits in the early stages of a disease when symptoms are still ambiguous. Because the tools can be used remotely, patients can reduce travel time and cost, especially if they live far from a clinic or have limited mobility.
- Provide easier access to diagnosis. At-home tools could help improve access to diagnostic information if they are self-administered, which can be particularly helpful in instances where a patient has health care access issues.
Challenges
- Limited testing. Some tools were designed for use at the clinic and researchers have conducted limited testing for at-home use. For example, quality control testing of at-home digital cognitive assessments lags behind those delivered in a clinical setting, but testing is critical to understand a tool’s reliability.
- Digital divide. At-home tools may be less useful and less widely adopted if patients do not understand how they work or do not have devices to access them. This challenge could contribute to disparities in diagnosis.
- Data privacy and security. Data could be sold, shared without consent, or accessed via data breaches, although data covered by the Health Insurance Portability and Accountability Act of 1996 are provided some additional safeguards.
Policy Context and Questions
- What are the possible policy implications for existing federal programs such as Medicare, Medicaid, and Social Security Insurance?
- What strategies, if any, might help enhance the benefits and use of at-home tools?
- What oversight or resources could help ensure the tools do not exacerbate health disparities and the digital divide?
- What safeguards could protect data privacy and security?
Selected GAO Work
Science & Tech Spotlight: Wearables, GAO-24-107303
Technology Assessment: Artificial Intelligence in Health Care, GAO-22-104629
Selected References
Ohman et al., “Current Advances in Digital Cognitive Assessment for Preclinical Alzheimer’s Disease,”Alzheimer’s and Dementia Diagnosis,Assessment and Disease Monitoring, (2021) doi: 10.1002/dad2.12217.
Adams et al., “Digital Technology in Movement Disorders: Updates, Applications, and Challenges,”Current Neurology and Neuroscience Reports,vol. 21, no. 4(2021).
For more information, contact Karen L. Howard, PhD at (202) 512-6888 or howardk@gao.gov.
