Medicaid Managed Care: Additional Federal Action Needed to Fully Leverage New Appeals and Grievances Data
Fast Facts
Because states pay Medicaid managed care plans per enrollee—rather than per service—there can be financial incentives for plans to deny or limit needed services.
As a safeguard, enrollees can appeal service denials and file grievances if dissatisfied. Starting in 2022, states were required to report some data on appeals and grievances to the Centers for Medicare & Medicaid Services annually.
But CMS's oversight is limited because it doesn't require states to report on service denials or appeal outcomes. Also, CMS hasn't made much progress on its plans to analyze and make the data publicly available.
Our 2 recommendations address these issues.
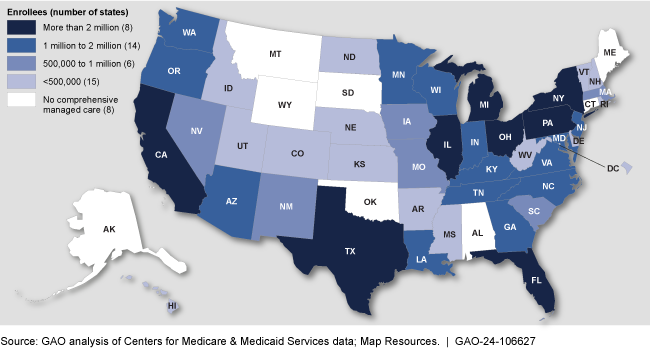
Over 70% of Medicaid enrollees receive services through managed care plans
Highlights
What GAO Found
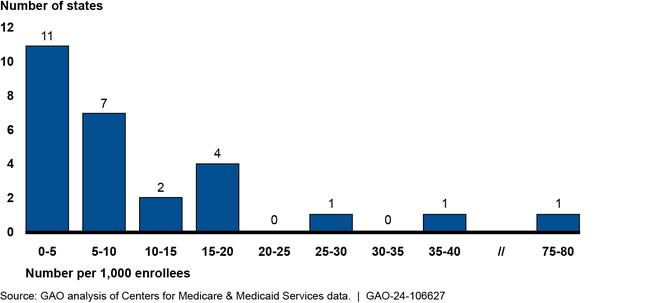
Managed care plans have some flexibility in determining when to authorize services for enrollees. Managed care enrollees may appeal denials of requested services and file grievances about any dissatisfaction not covered by an appeal. Data on appeals and grievances are an important tool for oversight of managed care, as they can help reveal quality and access issues. The first year of data from state annual managed care reports indicated that rates of appeals and grievances per 1,000 enrollees varied widely across states in 2022. Among other things, this could signal problems with access to needed services.
Medicaid Managed Care Plan Appeal Rates Across States with Reliable Appeals Data, Contract Year 2022
The Centers for Medicare & Medicaid Services (CMS) has begun taking steps to address limitations in the new appeals and grievances data. For example, as of December 2023, CMS had conducted technical assistance with seven states to address data gaps and inconsistencies. CMS has also outlined its intentions to use these data for oversight and to enhance transparency. However, GAO found:
- No data on outcomes or number of denials. CMS does not require states to report on the outcomes of enrollee appeals (e.g., whether a plan overturns its initial denial upon review) or the number of denials. These data elements are key to identifying potential problems with enrollee access to services.
- Delayed progress on planned actions to use the data. As of December 2023, CMS had made limited progress on its plans to analyze the data and make data available to the public. Taking these steps would help to inform CMS's data quality efforts and provide incentives for states to focus on quality.
By requiring states to report additional data and implementing planned steps to use the data, CMS would be better positioned to meet its goal to use the data to target program improvement, including around enrollee access to care.
Why GAO Did This Study
Over 70 percent of Medicaid enrollees receive services through managed care. Because there can be financial incentives for managed care plans to deny or limit services, appeal and grievance systems serve as a safeguard to protect enrollees. States are required to use appeals and grievances data to monitor managed care plans' performance. Beginning in 2022, states were also required to report certain managed care plan appeals and grievance data and other information to CMS annually.
GAO was asked to examine the new appeals and grievances data. This report (1) describes what the first-year data indicate about appeals and grievances, and (2) examines CMS's efforts to address any limitations in the data and its efforts to use the data for oversight.
GAO analyzed appeals and grievances data for state contract year 2022 across 35 states, and interviewed officials from five of these states, selected on the basis of geography and other factors. GAO also reviewed CMS documents, interviewed CMS officials, and assessed CMS's efforts against agency guidance.
Recommendations
GAO is making two recommendations to CMS: (1) to require states to report on appeal outcomes and number of denials; and (2) to implement planned actions for analyzing, using, and publicly posting the appeals and grievances data. The agency concurred with GAO's recommendations and noted plans to address them.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should require states to report on the outcomes of Medicaid managed care appeals (e.g., the extent to which they were decided in favor of enrollees) and number of denials. (Recommendation 1) |
HHS agreed with this recommendation and has begun taking steps to address it. As of September 2024, CMS has added appeal outcomes as required data elements to the Managed Care Program Annual Report (MCPAR), which will apply to all MCPARs beginning in June 2025. In addition, officials told us that CMS plans to add additional fields to capture the number of denials in Fall 2024 and that these fields will likely be required for MCPARs submitted starting in June 2026. We will review the MCPAR when CMS has added the denials fields and determine whether to close the recommendation at that time.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should implement its planned actions for analyzing the Medicaid managed care appeals and grievances data, using it for oversight, and making it publicly available. (Recommendation 2) |
HHS agreed with this recommendation and has begun taking steps to address it. In July 2024, CMS began posting states' Managed Care Program Annual Reports for performance year 2023 on Medicaid.gov and officials told us they will continue to post newly received reports on a regular basis. Additionally, in August 2024, CMS released Technical Guidance on data fields related to appeals and grievances to help states improve the consistency and quality of submitted data. This is a positive step toward making the data more complete and reliable so that it can be used for oversight. We will continue to monitor CMS's plans and actions for analyzing the appeals and grievances data and using it for oversight.
|
