Maternal Health: HHS Should Improve Assessment of Efforts to Address Worsening Outcomes
Fast Facts
Hundreds of women in the U.S. die each year from complications related to pregnancy and childbirth—a crisis exacerbated by COVID-19. The Department of Health and Human Services is working to address the crisis and meet long-term goals such as increasing women's access to high-quality maternal care.
As of September 2023, HHS hasn't determined how it'll measure progress toward achieving its maternal health goals. Following key performance measurement practices—such as setting near-term goals and establishing timeframes for results—would allow the agency to better understand if its efforts are effective. We recommended that HHS do so.
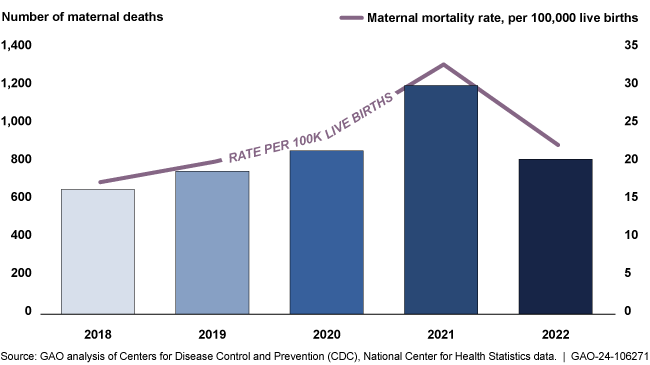
The number and rate of maternal deaths increased significantly during the COVID-19 pandemic
Highlights
What GAO Found
Maternal mortality and other adverse outcomes associated with pregnancy or childbirth worsened significantly in 2020 and 2021, as compared with 2018 and 2019, according to Department of Health and Human Services (HHS) data. Disparities in maternal health outcomes persisted during the pandemic for certain groups. For example, the maternal mortality rate among non-Hispanic, Black or African American women was about 2.5 times greater than non-Hispanic, White women during these years, according to GAO's analysis of HHS data.
Maternal Mortality by Race and Ethnicity, 2018 – 2022
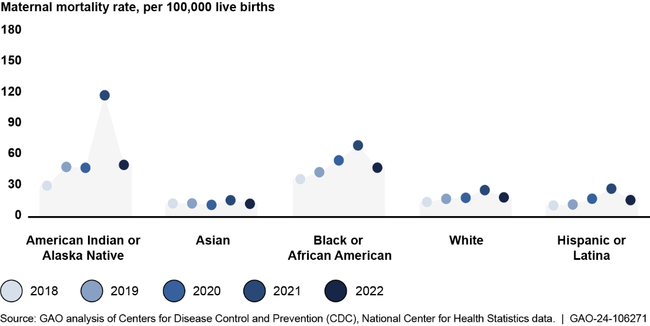
Notes: A maternal death is the death of a woman that occurs during or within 42 days of pregnancy from any cause related to or aggravated by the pregnancy or its management. All racial groups are not Hispanic or Latina; Hispanic or Latina women may be of any race.
The White House Blueprint for Addressing the Maternal Health Crisis was released in June 2022 in response to worsening outcomes and disparities. It highlights specific federal actions and outlines long-term goals for improving maternal health. HHS offices intend to develop a strategy for assessing the performance of these long-term goals. However, as of September 2023, HHS had not indicated whether the strategy will include key practices, such as establishing near-term goals and performance measures, to track the performance of their efforts . Doing so would allow HHS to better assess its efforts to improve maternal health.
The blueprint also identifies key maternal health efforts, such as the Centers for Disease Control and Prevention's (CDC) Perinatal Quality Collaborative program, which supports multidisciplinary teams implementing maternal health quality improvement initiatives. The CDC program has both long- and near-term goals, but the near-term goals lack quantitative targets, such as targets specifying the anticipated number of facilities participating in the Perinatal Quality Collaborative program. Establishing such targets would allow CDC to assess the program's progress to help improve maternal health outcomes.
Why GAO Did This Study
The U.S. is experiencing a maternal health crisis: it has one of the highest maternal mortality rates among high-income nations; increasing rates of complications from pregnancy or childbirth; and persistent disparities in such outcomes, according to HHS. GAO previously reported that the COVID-19 pandemic exacerbated maternal health outcomes and highlighted racial disparities.
The CARES Act includes a provision for GAO to report on its COVID-19 pandemic oversight efforts. GAO was also asked to review maternal health during the pandemic. Among other things, this report describes what available HHS data show about maternal health during COVID-19, and examines the extent to which HHS agencies have incorporated key practices to assess the performance of selected HHS maternal health efforts. GAO selected efforts based on factors such as the number of states in which teams implement the efforts. GAO reviewed HHS data for various years from 2016 through 2022 (based on availability), reviewed agency documentation, compared efforts against key practices, and interviewed HHS officials and stakeholders.
Recommendations
GAO is making two recommendations that (1) HHS ensure the Maternal Health Blueprint's performance measurement strategy follows key practices; and (2) CDC establish quantitative targets for the Perinatal Quality Collaborative program's near-term goals. HHS concurred with GAO's recommendations and noted plans to address them.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Department of Health and Human Services | The Secretary of Health and Human Services should ensure that the Office on Women's Health and Office of the Assistant Secretary for Planning and Evaluation performance strategy includes key performance management practices—including near-term goals with quantitative targets and time frames to define intended results and associated performance measures for the near-term goals—to assess the performance of HHS's maternal health efforts against the Maternal Health Blueprint's goals. (Recommendation 1) |
When we confirm what actions the agency has taken in response to this recommendation, we will provide updated information.
|
| Department of Health and Human Services | The Director of CDC should ensure that the Perinatal Quality Collaborative program establishes quantitative targets for its near-term goals to provide a basis for comparing planned and actual results. (Recommendation 2) |
When we confirm what actions the agency has taken in response to this recommendation, we will provide updated information.
|
