Veterans Community Care Program: VA Needs to Strengthen Its Oversight and Improve Data on Its Community Care Network Providers
Fast Facts
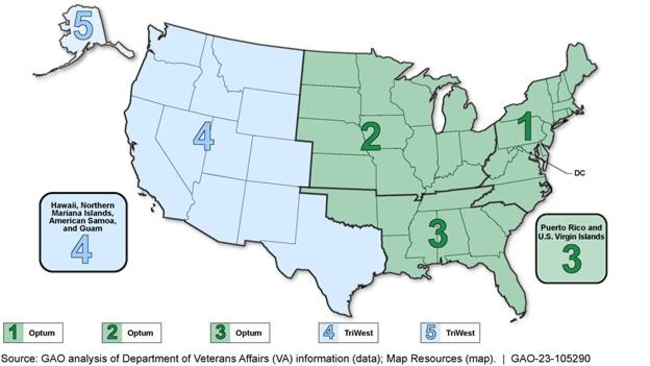
The VA uses two contractors to manage its regional networks of community providers, known as Community Care Networks, to deliver care to veterans. These contractors are responsible for maintaining adequate provider networks that meet two standards—maximum distances veterans may drive to community providers, and maximum wait times for appointments.
The VA monitors these contractors to ensure that they are complying with these standards. However, we found that these contractors did not submit all of the data that the VA needs to ensure that they are complying.
We recommended that the VA ensure that these contractors report complete data.
Map of VA Community Care Network Regions and Contractors (Optum and TriWest)
Highlights
What GAO Found
The Department of Veterans Affairs (VA) utilizes two contractors to manage its regional networks of community providers, called Community Care Networks, to deliver care to veterans under the Veterans Community Care Program. VA requires its contractors to meet two network adequacy standards that specify maximum drive-time distances and wait times for appointments.
VA monitors contractor compliance with network adequacy requirements by reviewing the contractors' analysis of claims data against the standards. VA officials determined the contractors generally met the standards for the period from April 2020 to May 2022. However, GAO found that VA's assessment was based on incomplete data, as the contractors did not include all claims. Further, VA was unaware of this, as it lacked a mechanism to ensure the contractors submitted complete data, limiting VA's performance assessment for Regions 1-4.
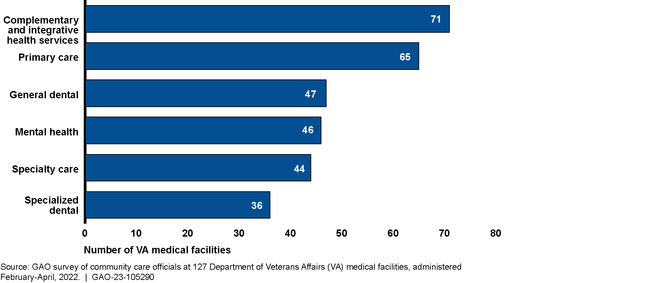
GAO's analysis of VA officials' responses from 127 of 138 VA medical facilities, and undercover calls to 80 community providers in Community Care Network Regions 1-4, revealed potential challenges with scheduling appointments. Specifically, officials cited challenges scheduling with certain types of providers within VA's routine appointment availability standard (care not deemed urgent or emergent by a VA provider). (See fig. below.) Responding officials noted concerns with insufficient VA facility staff to schedule appointments, and inaccurate provider information in VA's provider directory, including providers no longer participating in the network (also confirmed through GAO's undercover calls). These issues can delay appointment scheduling. GAO previously reported on these issues, and recommended in 2020 and 2021 that VA (1) direct its medical facilities to assess community care staffing and (2) improve controls to address risks related to inaccurate provider addresses, respectively. VA has taken some actions, but has not yet implemented these recommendations.
Number of VA Medical Facilities Reporting More than Half of Routine Appointments Scheduled within 30 Days by Care Type, April 2022
Why GAO Did This Study
Under the Veterans Community Care Program, VA's two Community Care Network contractors are responsible for maintaining provider networks that are adequate in size and have the capacity to ensure veterans' timely access to care.
GAO was asked to review VA's Community Care Networks. This report, for Community Care Network Regions 1-4, (1) describes how VA monitors contractor compliance with network adequacy standards and related requirements; (2) examines the extent to which VA's contractors are meeting network adequacy standards; and (3) examines the experiences of VA medical facility officials when scheduling routine appointments for veterans.
GAO reviewed documentation, such as the Community Care Network contracts, and network adequacy performance data and assessed VA's relevant processes. GAO conducted a survey of VA medical facility officials in Regions 1-4, and conducted covert calls to a non-generalizable sample of community providers. GAO also interviewed VA officials and contractor representatives.
Recommendations
In addition to reiterating prior recommendations related to staffing and fraud risks, GAO is making two new recommendations to VA: (1) ensure that contractors report complete performance data and (2) implement strategies to increase the accuracy of community provider information. VA concurred with the recommendations and identified steps it would take to implement them.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Department of Veterans Affairs | The Undersecretary for Health should ensure that Community Care Network contractors report complete claims data when calculating performance against VA's network adequacy standards. In cases where VA has made agreements with the contractors to exclude certain claims, those reasons should be clearly documented by VA. (Recommendation 1) |
The Veterans Health Administration (VHA) concurred with this recommendation, and in April 2023, stated that the Office of Integrated Veteran Care (IVC) developed a dashboard within VHA's Advanced Medical Cost Management Solution (AMCMS) system to be able to independently monitor network adequacy for both third party administrators, Optum and TriWest. As of October 2024, VA has provided documentation that shows it can review reported claims data from all five Community Care Network regions in AMCMS. In addition, VA officials stated that Optum began including appointment timeliness data in the network adequacy deliverable in August of 2021, and TriWest began including all applicable failed claims into the calculation for network adequacy in October 2022. Officials provided documentation that, where VA has agreed to the exclusion of claims, IVC has documented these agreed upon exclusions within the contract and associated quality assurance surveillance plan. Based on these actions, we are closing this recommendation.
|
| Department of Veterans Affairs | The Undersecretary for Health should review its processes for monitoring the accuracy and completeness of contractor-submitted provider data in PPMS and implement strategies under current or future contracts to increase the accuracy of provider information stored in PPMS. For example, VA could require the contractors to use proactive processes to ensure data accuracy. (Recommendation 2) |
The Veterans Health Administration (VHA) concurred with this recommendation and has provided information on strategies it is using to increase the accuracy of community provider information in the Provider Profile Management System (PPMS). First, in February 2024, VHA provided documentation confirming that it has hired seven full time employees to create a permanent PPMS Data Management Team to conduct multi-pronged audits using contractor provider portal data from Optum to compare to data contained in PPMS. According to VHA officials, these audits will be completed monthly into the next generation community care network contracts and will allow VHA to identify and resolve data transmission problems. For TriWest, VHA stated in June 2024 that the PPMS Data team extracts a file from PPMS to send to the contractor to identify and resolve discrepancies weekly. Officials said these audits will continue into the next generation contracts if similar data is used. VHA provided documentation confirming both audit processes. Second, in April 2023, VHA officials stated they've added fields to PPMS to note provider availability and shares these reports with both contractors to take action when appropriate. Last, officials said the PPMS Data team developed and provided training to local community care offices. According to VHA provided documentation, the training included information on how to find a provider in PPMS, how to update provider availability, how to add custom notes to a provider's profile, and how to save custom searches, among other things. Based on VHA's actions, we are closing this recommendation.
|
