Artificial Intelligence in Health Care: Benefits and Challenges of Technologies to Augment Patient Care
Fast Facts
Artificial Intelligence tools show promise for improving health care. They can help predict health trajectories, recommend treatments, and automate administrative tasks. Challenges associated with these tools include:
Transparency: If a medical provider doesn't know how a tool works, it could reduce trust in the tool.
Bias: Limitations and bias in data can reduce the safety and effectiveness of AI tools.
Data: Obtaining the high-quality data needed to create effective AI tools can be difficult.
We offer policy options—such as improving data access, establishing best practices, and more—to address these and other challenges we found.
AI generates information for health care providers to help them better care for patients and be more efficient.
Highlights
What GAO Found
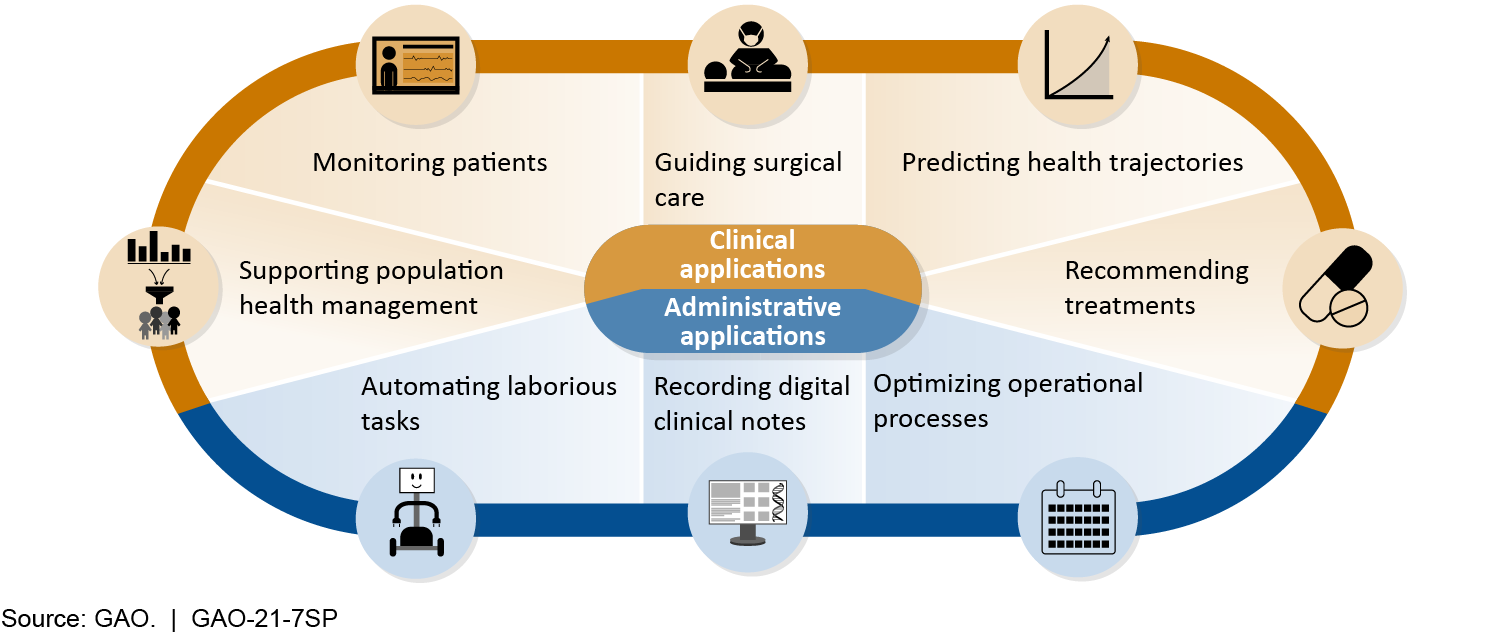
Artificial Intelligence (AI) tools have shown promise for augmenting patient care in the following two areas:
- Clinical AI tools have shown promise in predicting health trajectories of patients, recommending treatments, guiding surgical care, monitoring patients, and supporting population health management (i.e., efforts to improve the health outcomes of a community). These tools are at varying stages of maturity and adoption, but many we describe, with the exception of population health management tools, have not achieved widespread use.
- Administrative AI tools have shown promise in reducing provider burden and increasing efficiency by recording digital notes, optimizing operational processes, and automating laborious tasks. These tools are also at varying stages of maturity and adoption, ranging from emerging to widespread.
GAO identified the following challenges surrounding AI tools, which may impede their widespread adoption:
- Data access. Developers experience difficulties obtaining the high-quality data needed to create effective AI tools.
- Bias. Limitations and bias in data used to develop AI tools can reduce their safety and effectiveness for different groups of patients, leading to treatment disparities.
- Scaling and integration. AI tools can be challenging to scale up and integrate into new settings because of differences among institutions and patient populations.
- Lack of transparency. AI tools sometimes lack transparency—in part because of the inherent difficulty of determining how some of them work, but also because of more controllable factors, such as the paucity of evaluations in clinical settings.
- Privacy. As more AI systems are developed, large quantities of data will be in the hands of more people and organizations, adding to privacy risks and concerns.
- Uncertainty over liability. The multiplicity of parties involved in developing, deploying, and using AI tools is one of several factors that have rendered liability associated with the use of AI tools uncertain. This may slow adoption and impede innovation.
GAO developed six policy options that could help address these challenges or enhance the benefits of AI tools. The first five policy options identify possible new actions by policymakers, which include Congress, elected officials, federal agencies, state and local governments, academic and research institutions, and industry. The last is the status quo, whereby policymakers would not intervene with current efforts. See below for details of the policy options and relevant opportunities and considerations.
Policy Options to Address Challenges or Enhance Benefits of AI to Augment Patient Care
| Policy Option | Opportunities | Considerations |
|
Collaboration (report p. 32)
|
|
|
|
Data Access (report p. 33)
|
|
|
|
Best Practices (report p. 34)
|
|
|
|
Interdisciplinary Education (report p. 35)
|
|
|
|
Oversight Clarity (report p. 36)
|
|
|
|
Status quo (report p. 37) Policymakers could maintain the status quo (i.e., allow current efforts to proceed without intervention). |
|
|
Source: GAO.
Why GAO did this study
The U.S. health care system is under pressure from an aging population; rising disease prevalence, including from the current pandemic; and increasing costs. New technologies, such as AI, could augment patient care in health care facilities, including outpatient and inpatient care, emergency services, and preventative care. However, the use of AI-enabled tools in health care raises a variety of ethical, legal, economic, and social concerns.
GAO was asked to conduct a technology assessment on the use of AI technologies to improve patient care, with an emphasis on foresight and policy implications. This report discusses (1) current and emerging AI tools available for augmenting patient care and their potential benefits, (2) challenges surrounding the use of these tools, and (3) policy options to address challenges or enhance benefits of the use of these tools.
GAO assessed AI tools developed for or used in health care facilities; interviewed a range of stakeholder groups including government, health care, industry, academia, and a consumer group; convened a meeting of experts in collaboration with the National Academy of Medicine; and reviewed key reports and scientific literature. GAO is identifying policy options in this report.
For more information, contact Karen L. Howard at (202) 512-6888 or howardk@gao.gov.
