Medicaid Long-Term Services and Supports: Access and Quality Problems in Managed Care Demand Improved Oversight
Fast Facts
Medicaid spends about a third of its budget on long-term services and supports for adults and children with disabilities and chronic conditions. Over half of states contract with managed care organizations to provide those services.
We examined 6 states, each of which reported finding significant problems with the quality of care provided through these contracts. In some cases, the problems led to patient injury or neglect. This suggests that problems may be widespread, raising concerns given gaps we found in monitoring and oversight.
Our recommendations include drafting a national oversight strategy.
Needs of Medicaid Beneficiaries That May Be Addressed with Long-Term Services and Supports
Highlights
What GAO Found
At the state and federal levels, GAO found weaknesses in the oversight of Medicaid managed long-term services and supports (MLTSS), which assist individuals with basic needs like bathing or eating.
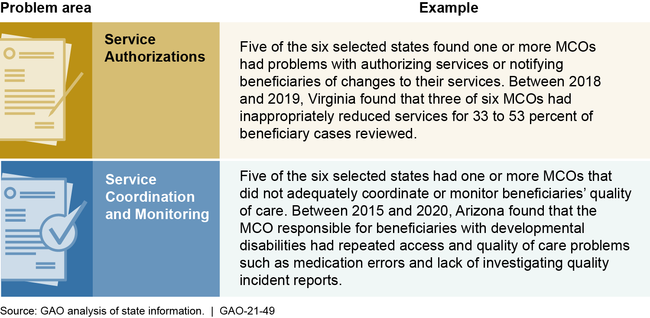
Through various monitoring approaches, six selected states identified significant problems in their MLTSS programs with managed care organization (MCO) performance of care management, which includes assessing beneficiary needs, authorizing services, and monitoring service provision to ensure quality and access to care. State efforts may not be identifying all care management problems due to limitations in the information they use to monitor MCOs, allowing some performance problems to continue over multiple years.
Performance Problems in Managed Care Organization (MCO) Care Management, Identified by Selected States
GAO found that the Centers for Medicare & Medicaid Services' (CMS) oversight of state implementation of its 2016 requirements, and of access and quality in MLTSS more broadly, was limited. This hinders the agency's ability to hold states and MCOs accountable for quality and access problems beneficiaries may face.
- Oversight did not detect quality and access problems. GAO identified cases where CMS learned about problems not through its regular oversight, but instead from beneficiary complaints, media reports, or GAO. CMS officials said that states had not reported these problems to the agency.
- Lack of national oversight strategy and assessment of problems in MLTSS. Weaknesses in oversight reflect a broader area of concern—namely, that CMS lacks a strategy for oversight. CMS also has not assessed the nature and extent of access and quality problems across states. Without a strategy and more robust information, CMS risks being unable to identify and help address problems facing beneficiaries. As of July 2020, CMS had convened a new workgroup focused on MLTSS oversight, though the goals and time frames for its work were unclear.
Why GAO Did This Study
An increasing number of states are using managed care to deliver long-term services and supports in their Medicaid programs, thus delegating decisions around the amounts and types of care beneficiaries receive to MCOs. Federal guidance requires that MLTSS programs include monitoring procedures to ensure the appropriateness of those decisions for this complex population, which includes adults and children who may have physical, cognitive, and mental disabilities.
GAO was asked to review care management in MLTSS programs. Among other things, this report examines state monitoring of care management, and CMS oversight of state implementation of 2016 requirements related to MLTSS quality and access. GAO examined documentation of monitoring procedures and problems identified in six states selected for variation in program age and location. GAO reviewed federal regulations and oversight documents, interviewed state and federal Medicaid officials, and assessed CMS's policies and procedures against federal internal control standards.
Recommendations
GAO is making two recommendations to CMS to (1) develop a national strategy for overseeing MLTSS, and (2) assess the nature and prevalence of MLTSS quality and access problems across states. CMS did not concur with the recommendations. GAO maintains the recommendations are warranted, as discussed in this report.
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services |
Priority Rec.
The Administrator of CMS should develop and implement a national strategy for monitoring MLTSS programs and ensuring that states and MCOs resolve identified problems. Among other things, this strategy should address state implementation of beneficiary protection and monitoring requirements. (Recommendation 1) |
CMS did not concur with our recommendation. However, in June 2022 CMS took a number of steps to enhance oversight. CMS issued a new technical assistance toolkit for states to use in overseeing MLTSS programs, as well as an updated Managed Care Program Annual Report template, which requires states to report a number of different data on MLTSS, including on beneficiary protection systems and on certain appeals and grievances. As of February 2024, CMS reported that it continues to assess states' submission of the annual reports for completeness and reasonableness. Once CMS finds that data is sufficiently complete it will establish a strategy for analyzing and following up on specific information and for assessing the nature of access and quality issues identified. The agency indicated that it is reassessing the use of the appeals and grievance reporting template and may combine it with another template being tested to produce a more effective single data collection tool. We will continue to monitor CMS actions on this recommendation, including any evidence of a strategy for resolving identified problems with state MLTSS programs.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should assess the nature and prevalence of MLTSS access and quality problems across states. (Recommendation 2) |
CMS did not concur with our recommendation. However, in June 2022 CMS issued an updated Managed Care Program Annual Report template that required states to report on the performance of managed care organizations and any sanctions or corrective actions issued. As of February 2024, CMS reported that it continues to assess states' submission of the annual reports for completeness and reasonableness. Once CMS finds that data is sufficiently complete it will establish a strategy for analyzing and following up on specific information and for assessing the nature of access and quality issues identified. The agency indicated that it is reassessing the use of the appeals and grievance reporting template and may combine it with another template being tested to produce a more effective single data collection tool. We will continue to monitor CMS actions on this recommendation, including any evidence of a strategy for resolving identified problems with state MLTSS programs. 2/23/24
|
