Medicare: Additional Reporting on Key Staffing Information and Stronger Payment Incentives Needed for Skilled Nursing Facilities [Reissued with revisions on Aug. 10, 2021.]
Fast Facts
Medicare spent nearly $28 billion in 2019 on short-term care for 1.5 million beneficiaries in skilled nursing facilities after hospital stays.
Research indicates low nurse staffing can lead to potentially preventable re-hospitalizations. We found most facilities had a registered nurse on site 8 hours a day, as required. A federal study identified the nurse staffing levels needed to avoid care quality problems, but only 1 in 4 facilities met them.
We estimated Medicare spent over $5 billion in 2018 on re-hospitalizations; it can cut payments by up to 2% for facilities that don't reduce re-hospitalizations.
We recommended actions to improve care.

On August 10, 2021, this report was corrected to display the first page of written comments from the Department of Health and Human Services, which appears on page 52.
Highlights
What GAO Found
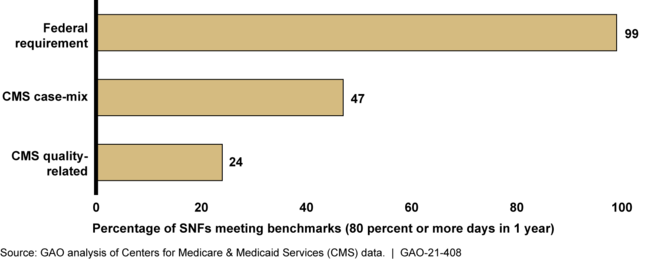
Medicare covers short-term care for residents in about 15,500 skilled nursing facilities (SNF) after a hospital stay. GAO's analysis of 2019 staffing data found that almost all SNFs frequently met a federal requirement for a registered nurse (RN) on site for 8 hours per day. Fewer SNFs frequently met two other staffing measures that specify different numbers of nursing hours per resident per day. For example, about half of SNFs frequently met Centers for Medicare & Medicaid Services (CMS) case-mix measures—hours worked per resident that vary based on the medical needs of each SNF's residents—that CMS uses to set SNF staffing ratings. Further, about one-quarter of SNFs frequently met staffing thresholds for minimum RN and total nurse staffing that a CMS staffing study identified as needed to avoid quality problems. SNFs are not subject to these quality thresholds for ratings or as requirements, but many stakeholders have recommended that they be used as SNF staffing thresholds.
Percent of Skilled Nursing Facilities (SNFs) That Met Registered (RN) Nurse Staffing Requirement or Measures, 2019
CMS reports certain key staffing information—such as RN overall staffing hours—on its Care Compare website, but does not report other important information. For example, GAO found that average RN staffing hours decreased about 40 percent on weekends, but CMS does not directly report this information. This limits the ability of beneficiaries to make informed choices among SNFs when choosing a facility.
GAO estimated that in 2018 Medicare spent over $5 billion on critical incidents that CMS defines as potentially preventable—which are mostly about 377,000 hospital readmissions occurring within 30 days of the SNF admission. Current law directs CMS to make reductions of up to 2 percent to certain SNFs' payments to incentivize them to improve care, but does not address additional reductions. Experts have noted that payment incentives under current law may not be sufficient to motivate SNFs to improve their staffing, which in turn could lead to reductions in critical incidents. Without stronger payment incentives, Medicare is unlikely to reduce the billions in spending on potentially preventable critical incidents or the patient harm that can occur from them.
Why GAO Did This Study
In 2019, Medicare spent nearly $28 billion on care provided to 1.5 million beneficiaries in SNFs—a type of nursing facilty that provides residents short-term rehabilitation care after a hospital stay rather than long-term nursing home care that Medicare does not cover. SNFs must meet federal standards to participate in Medicare. CMS rates SNFs on factors such as staffing and quality of care and publishes its ratings on the Care Compare website.
GAO was asked to examine SNF staffing and rates of critical incidents. This report examines (among other objectives): SNF performance on staffing measures, CMS reporting of staffing information on Care Compare, and Medicare payments for critical incidents. GAO analyzed CMS staffing and critical incidents data, information on Care Compare, and Medicare claims data for 2018 and 2019. GAO also interviewed CMS officials and other stakeholders such as key researchers and beneficiary groups.
Reissued with revisions on Aug. 10, 2021.
On August 10, 2021, this report was corrected to display the first page of written comments from the Department of Health and Human Services, which appears on page 52.Recommendations
Congress should consider directing the Secretary of the Department of Health and Human Services to implement appropriate payment reductions for SNFs that generate Medicare spending on potentially preventable critical incidents. GAO is making three recommendations, including that CMS report more staffing information on Care Compare. HHS agreed to report weekend decreases in nurse staffing levels, but did not agree to report minimum nurse staffing thresholds needed to ensure quality of care. GAO continues to believe both are important, as discussed in the report.
Matter for Congressional Consideration
| Matter | Status | Comments |
|---|---|---|
| Congress should consider directing the Secretary of HHS to implement additional reductions in payments to SNFs that generate Medicare spending on potentially preventable critical incidents—hospital readmissions and ER visits that occur within 30 days of the SNF admissions—either through the SNF Value-Based Purchasing program or some other vehicle, including, as needed, making any appropriate modifications to enable HHS to take action. | No congressional action has been taken to implement additional payment reductions to SNFs that generate Medicare spending on potentially preventable critical incidents as of March 1, 2024. As we reported, Medicare spent over $5 billion in 2018 on critical incidents that CMS defines as potentially preventable. Under current law, CMS is directed to make reductions of up to 2 percent to certain SNFs' payments to incentivize them to improve care, but additional reductions are not authorized. Without congressional action, Medicare is unlikely to reduce the billions in spending on potentially preventable critical incidents or the patient harm that can occur from them. |
Recommendations for Executive Action
| Agency Affected | Recommendation | Status |
|---|---|---|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should report weekend decreases in RN and total nurse staffing levels on the Care Compare website. (Recommendation 1) |
CMS concurred with the recommendation to report weekend decreases in RN and total nurse staffing levels on the Care Compare website. On January 7, 2022, CMS published a memorandum detailing its plan to begin posting information on the level of total nurse and registered nurse staffing on weekends provided by each nursing home over each quarter. As of May 2022, that information is incorporated into the Care Compare website. As a result, beneficiaries have the improved ability to make informed choices among SNFs when choosing a facility for their care.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should report minimum RN and total nurse staffing thresholds below which SNF residents are at increased risk of quality problems—such as thresholds that are similar to those identified in the CMS staffing study—on the Care Compare website. (Recommendation 2) |
CMS has taken steps to address our recommendation. Specifically, in April 2022, CMS stated that it intends to propose minimum staffing standards for staffing adequacy that nursing homes would be required to meet. CMS noted that it will conduct a new research study to help determine the level and type of staffing needed to ensure safe and quality care and expects to issue proposed rules within a year with stakeholder input to inform these decisions. We will update the status of this recommendation when we receive additional information. As of March 2023, CMS has not issued a proposed rule on this issue.
|
| Centers for Medicare & Medicaid Services | The Administrator of CMS should assess the feasibility of incorporating into the Five-Star System staffing ratings information on weekend decreases in RN and total nurse staffing levels, and minimum RN and total nurse staffing thresholds below which SNF residents are at increased risk of quality problems—such as those that were identified in the CMS staffing study. (Recommendation 3) |
HHS concurred with the recommendation to assess the feasibility of incorporating information on weekend RN and total nurse staffing levels into the Five-Star System staffing ratings. On July 7, 2022, CMS published an update to its Nursing Home Five Star Quality Rating System, which adds the measures of weekend RN and total nurse staffing to the staffing rating domain to encourage facilities to increase nurse staffing on weekends. As a result, beneficiaries have the improved ability to make informed choices among SNFs when choosing a facility for their care.
|
