Medicaid: Actions Needed to Mitigate Billions in Improper Payments and Program Integrity Risks
Fast Facts
The Medicaid program helped provide health care to an estimated 73 million people in fiscal 2017 at a cost of about $596 billion. This joint federal and state program continues to grow, and remains on our high risk list due to concerns about the adequacy of federal oversight and the program's vulnerability to fraud.
This testimony focuses on the major risks to the integrity of Medicaid. Efforts needed to strengthen oversight include:
expansion of a national Medicaid data system that will allow comparisons across states,
a national anti-fraud strategy,
greater collaboration between state and federal auditors.
Growth Trends in Medicaid Spending by Eligibility Group
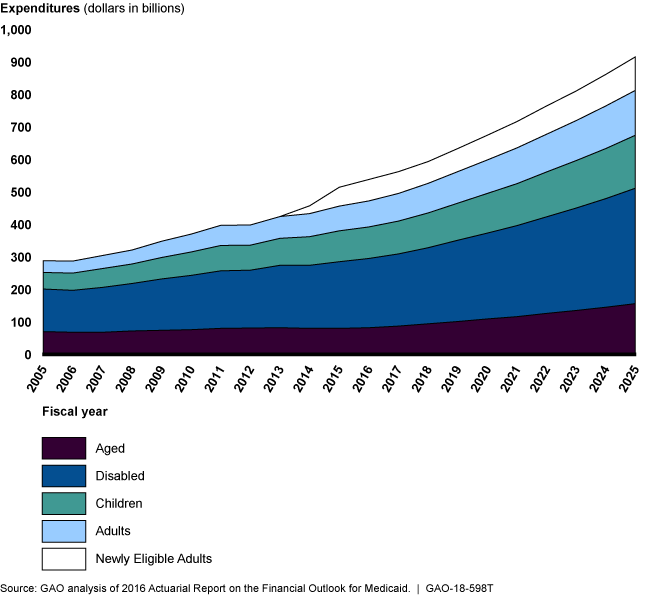
The number of recipients is growing. The 5 groups are the aged, disabled, children, adults, and newly eligible adults.
Highlights
What GAO Found
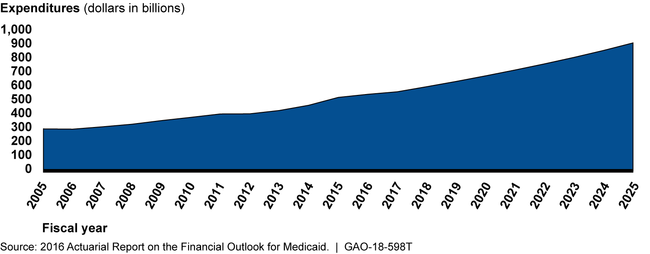
GAO's work has identified three broad areas of risk in Medicaid that also contribute to overall growth in program spending, projected to exceed $900 billion in fiscal year 2025.
1) Improper payments, including payments made for services not actually provided. Regarding managed care payments, which were nearly half (or $280 billion) of Medicaid spending in fiscal year 2017, GAO has found that the full extent of program risk due to overpayments and unallowable costs is unknown.
2) Supplemental payments, which are payments made to providers—such as local government hospitals—that are in addition to regular, claims-based payments made to providers for specific services. These payments totaled more than $48 billion in fiscal year 2016 and in some cases have shifted expenditures from the states to the federal government.
3) Demonstrations, which allow states to test new approaches to coverage. Comprising about one-third of total Medicaid expenditures in fiscal year 2015, GAO has found that demonstrations have increased federal costs without providing results that can be used to inform policy decisions.
Actual and Projected Growth Trends in Total Medicaid Spending
GAO's work has recommended numerous actions to strengthen oversight and manage program risks.
- Improve data. The Centers for Medicare & Medicaid Services (CMS), which oversees Medicaid, needs to make sustained efforts to ensure Medicaid data are timely, complete, and comparable from all states, and useful for program oversight. Data are also needed for oversight of supplemental payments and ensuring that demonstrations are meeting their stated goals.
- Target fraud. CMS needs to conduct a fraud risk assessment for Medicaid, and design and implement a risk-based antifraud strategy for the program.
- Collaborate. There is a need for a collaborative approach to Medicaid oversight. State auditors have conducted evaluations that identified significant improper payments and outlined deficiencies in Medicaid processes that require resolution.
Why GAO Did This Study
Medicaid, a joint federal-state health care program overseen by CMS, is a significant component of federal and state budgets, with total estimated expenditures of $596 billion in fiscal year 2017.
Medicaid allows significant flexibility for states to design and implement program innovations based on their unique needs. The resulting diversity of the program and its size, make the program particularly challenging to oversee at the federal level and also vulnerable to improper payments. In fiscal year 2017, estimated improper payments were $36.7 billion in Medicaid, up from $29.1 billion in fiscal year 2015. Further, the Medicaid program accounted for about 26 percent of the fiscal year 2017 government-wide improper payment estimate.
This testimony focuses on the (1) major risks to the integrity of the Medicaid program, and (2) actions needed to manage these risks. This testimony draws on GAO's reports issued between November 2012 and May 2018 on the Medicaid program.
Recommendations
As a part of this body of work, GAO has made 83 recommendations to address shortcomings in Medicaid oversight and suggested four matters for congressional consideration. The Department of Health and Human Services and CMS have generally agreed with these recommendations and have implemented 25 of them. GAO will continue to monitor implementation of the remaining recommendations.
