Health Care Fraud: Information on Most Common Schemes and the Likely Effect of Smart Cards
Highlights
What GAO Found
GAO's review of 739 health care fraud cases that were resolved in 2010 showed the following:
- About 68 percent of the cases included more than one scheme with 61 percent including two to four schemes and 7 percent including five or more schemes.
- The most common health care fraud schemes were related to fraudulent billing, such as billing for services that were not provided (about 43 percent of cases) and billing for services that were not medically necessary (about 25 percent).
- Other common schemes included falsifying records to support the fraud scheme (about 25 percent), paying kickbacks to participants in the scheme (about 21 percent), and fraudulently obtaining controlled substances or misbranding prescription drugs (about 21 percent).
- Providers were complicit in 62 percent of the cases, and beneficiaries were complicit in 14 percent of the cases.
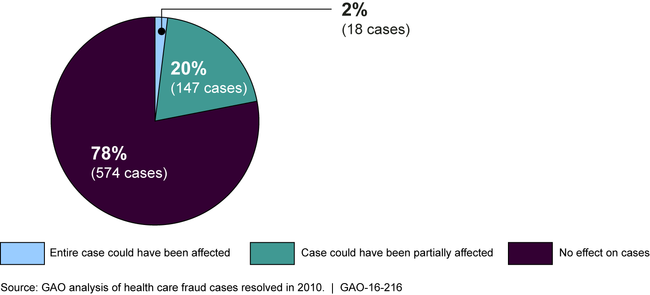
GAO's analysis found that the use of smart cards could have affected about 22 percent (165 cases) of cases GAO reviewed in which the entire or part of the case could have been affected because they included schemes that involved the lack of verification of the beneficiary or provider at the point of care. However, in the majority of cases (78 percent), smart card use likely would not have affected the cases because either beneficiaries or providers were complicit in the schemes, or for other reasons. For example, the use of cards would not have affected cases in which the provider misrepresented the service (as in billing for services not medically necessary), or when the beneficiary and provider were not directly involved in the scheme (as in illegal marketing of prescription drugs).
Percentage of 2010 Health Care Fraud Cases Reviewed That Could Have Been Affected by Use of Smart Card Technology
Why GAO Did This Study
While there have been convictions for multimillion dollar schemes that defrauded federal health care programs, there are no reliable estimates of the magnitude of fraud within these programs or across the health care industry. In some fraud cases, individuals have billed federal health care programs or private health insurance by using a beneficiary's or provider's identification information without the beneficiary's or provider's knowledge. One idea to reduce the ability of individuals to commit this type of fraud is to use electronically readable card technology, such as smart cards. Proponents say that these cards could reduce fraud by verifying that the beneficiary and the provider were present at the point of care.
GAO was asked to identify and categorize schemes found in health care fraud cases. This report describes (1) health care fraud schemes and their prevalence among cases resolved in 2010 and (2) the extent to which health care fraud schemes could have been affected by the use of smart card technology. GAO reviewed reports on health care fraud and smart card technology and reviewed court documents for 739 fraud cases resolved in 2010 obtained for a related 2012 GAO report on health care fraud. GAO is not making any recommendations.
The Department of Health and Human Services and the Department of Justice provided technical comments on a draft of this report, which GAO incorporated as appropriate.
For more information, contact Kathleen M. King at (202) 512-7114 or kingk@gao.gov.