COVID-19 Potential Impact on Prisons’ Populations and Health Care Costs
Recent reports of COVID-19 (coronavirus) outbreaks in prisons have raised concerns about health risks for inmates, and the availability and cost of care in prisons. The Federal Bureau of Prisons currently cares for about 143,000 inmates in 122 facilities.
In today’s WatchBlog, we look at steps the Federal Bureau of Prisons has taken to address health concerns, and our work on inmate health and healthcare costs.
Prison inmates may face higher health risks from COVID-19
Social distancing is meant to promote health and prevent the spread of COVID-19. But in prisons, people are in close contact and cannot practice social distancing—potentially allowing the coronavirus to spread more quickly. Inmates may be more at risk of exposure as a result.
In addition, the health profiles of many prisoners put them at higher risk for severe illness and higher mortality rate if infected with the virus. According to the Centers of Disease Control (CDC), people of any age—and older adults, in particular—who have serious underlying medical conditions may be at higher risk for severe illness from COVID-19. During our review of factors that contributed to higher Bureau health care costs, we found that the prison population includes:
- Older inmates — In 2016, about 12% of Bureau inmates were 55 years of age or older. Our analysis found that the average age of inmates increased each year from fiscal years 2009 to 2016. If this trend continued, it is likely that a higher percentage of inmates are of an age that puts them more at risk of serious health issues if they contract COVID-19.
- Inmates have relatively poorer health— During our review of the Bureau’s healthcare costs, officials said that inmates generally enter the system with more acute health needs due to limited access to care. Inmates also tend to have higher rates of infectious diseases—such as hepatitis C and HIV/AIDS from engaging in risky behavior like substance abuse—and chronic conditions such as cancer that can persist throughout incarceration. For example, the Bureau estimated that there were approximately 20,000 inmates infected with hepatitis C. Similarly, rates of chronic health and infection disease are 7 times higher for inmates than that of the general population, according to the Council of State Governments Justice Center. Underlying health conditions have been connected with COVID-19 related hospitalizations and deaths.
How is the Bureau protecting prison inmates?
In response to health concerns, the Bureau announced it would modify operations to help mitigate the spread of the coronavirus in prisons. As of May 2020, changes include:
- Suspending all social and legal visits for 30 days unless a request for an in-person attorney visit is approved by the local institution, and restricting the transfer of prisoners between facilities and systems (except in limited circumstances, such as federal or state court case processing)
- Screening staff in areas where there is sustained transmission of the virus and at medical referral centers
- Screening inmates newly arriving at a facility and quarantining those who were likely exposed to the virus
- Testing and isolating inmates who show symptoms of COVID-19.
- Maximizing social distancing, such as staggering meal and recreation times as much as is practicable
- Granting certain eligible prisoners home confinement
What does this mean for the Bureau’s healthcare costs?
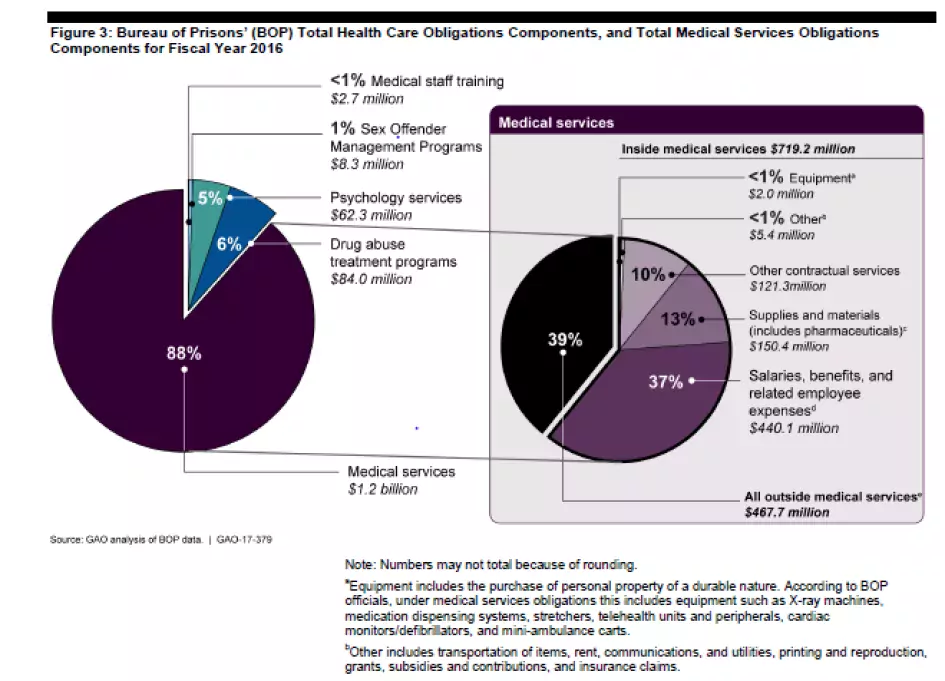
In our review of the Bureau’s health care costs, we found that medical services comprised 88% or $1.2 billion of the Bureau’s total health care obligations in 2016. The coronavirus could add to these costs. For example, the Bureau will need to purchase additional equipment and supplies, such a masks, gloves, thermometers, and ventilators. Total salaries and benefits expenditures could increase because Bureau medical staff may be needed to work overtime to screen for the virus and treat inmates. Further, outside medical care costs could increase if Bureau medical facilities are unable to manage the number of ill inmates and they must be sent to private physicians or hospital for care.
Check out our report to learn more about the factors that drive the Bureau’s healthcare costs and the initiatives it has in place to control them.
Comments on GAO’s WatchBlog? Contact blog@gao.gov
GAO Contacts
Related Products

GAO's mission is to provide Congress with fact-based, nonpartisan information that can help improve federal government performance and ensure accountability for the benefit of the American people. GAO launched its WatchBlog in January, 2014, as part of its continuing effort to reach its audiences—Congress and the American people—where they are currently looking for information.
The blog format allows GAO to provide a little more context about its work than it can offer on its other social media platforms. Posts will tie GAO work to current events and the news; show how GAO’s work is affecting agencies or legislation; highlight reports, testimonies, and issue areas where GAO does work; and provide information about GAO itself, among other things.
Please send any feedback on GAO's WatchBlog to blog@gao.gov.