Public Health Emergencies: Data Management Challenges Impact National Response
Fast Facts
Public health emergencies evolve quickly, but public health entities lack the ability to share new data and potentially life-saving information in real-time—undermining the nation's ability to respond quickly.
To address this, the federal government must overcome three major challenges—specifically, the lack of:
- Common standards for collecting data (e.g., patient characteristics)
- "Interoperability" (meaning not all data systems work together)
- Public health IT infrastructure (the hardware, software, networks, and policies that would enable the reporting and sharing of data)
This snapshot discusses our related work and recommendations.

Highlights
Public health emergencies evolve quickly, but public health entities lack the ability to share new data and potentially life-saving information in near real-time. To address this, the federal government must overcome 3 major challenges in how it manages public health data. GAO has made a number of recommendations to help address these challenges. However, many of these recommendations have not been implemented.
The Big Picture
Longstanding challenges in the federal government’s management of public health data undermine the nation’s ability to quickly respond to public health emergencies like COVID-19 and monkeypox. These challenges include the lack of:
- common data standards—requirements for public health entitles to collect certain data elements, such as patient characteristics (e.g., name, sex, and race) and clinical information (e.g., diagnosis and test results) in a specific way;
- interoperability—the ability of data collection systems to exchange information with and process information from other systems; and
- public health IT infrastructure—the computer software, hardware, networks, and policies that enable public health entities to report and retrieve data and information.
Over 15 years ago, federal law mandated that the Department of Health and Human Services (HHS) establish a national public health situational awareness network with a standardized data format. This network was intended to provide secure, near real-time information to facilitate early detection of and rapid response to infectious diseases.
However, the federal government still lacks this needed network and has not yet overcome the challenges identified in previous GAO reviews. Having near real-time access to these data could significantly improve our nation’s preparedness for public health emergencies and potentially save lives.
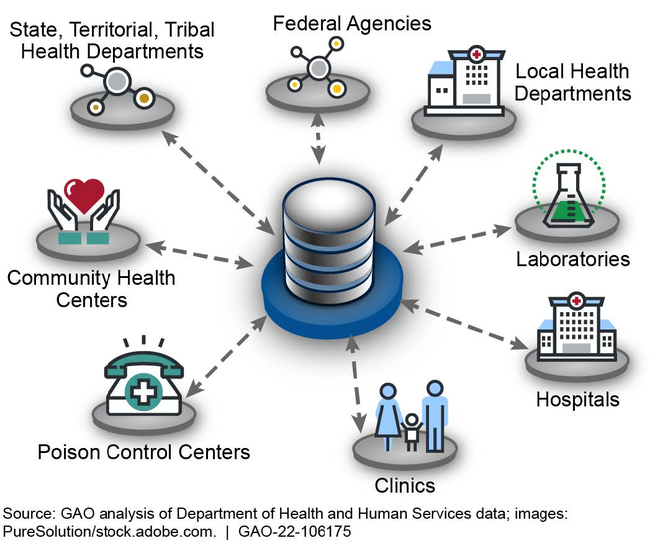
Without the network, federal, state, and local health departments, hospitals, and laboratories are left without the ability to easily share health information in real-time to respond effectively to diseases.
Illustration of a National Public Health Situational Awareness Network
What GAO’s Work Shows
GAO’s prior work identified three broad challenges to public health data management and recommended actions for improvement.
1. Common Data Standards
To ensure that information can be consistently reported, compared, and analyzed across jurisdictions, public health entities need a standardized data format. Due to the lack of common data standards, information reported by states about COVID-19 case counts was inconsistent. This in turn complicated the ability of the Centers for Disease Control and Prevention (CDC) to make comparisons. Public health representatives also noted challenges in collecting complete demographic data. This made it difficult to identify trends in COVID-19 vaccinations and the number of doses administered. Although CDC had intended to implement data standards, its strategic plan did not articulate specific actions, roles, responsibilities, and time frames for doing so.
- We recommended that HHS establish an expert committee for data collection and reporting standards by engaging with stakeholders (e.g., health care professionals from public and private sectors). This committee should review and inform the alignment of ongoing data collection and reporting standards related to key health indicators.
- We recommended that CDC define specific action steps and time frames for its data modernization efforts.
2. Interoperability among Public Health IT Systems
The inability to easily exchange information across data collection and other data systems creates barriers to data sharing and additional burdens on entities that collect and transmit data. During the early stages of COVID-19, the lack of IT system interoperability caused health officials and their key stakeholders (e.g., hospitals) to manually input data into multiple systems. In addition, some state health departments could not directly exchange information with CDC via an IT system. This led to longer time frames for CDC to receive the data they needed to make decisions on the COVID-19 response.
- We recommended that, as part of planning for the public health situational awareness network, HHS should ensure the plan includes how standards for interoperability will be used.
3. Lack of a Public Health IT Infrastructure
The timeliness and completeness of information that is shared during public health emergencies can be impeded by the absence of a public health IT infrastructure. During the early stages of COVID-19, some states had to manually collect, process, and transfer data from one place to another. For example, a state official described having to fax documents, make copies, and physically transport relevant documents. The official noted by establishing a public health IT infrastructure, such as the network HHS was mandated to create, errors would be reduced. To help mitigate challenges in data management for COVID-19, HHS launched the HHS Protect platform in April 2020. However, we reported that public health and state organizations raised questions about the completeness and accuracy of some of the data.
- We recommended that HHS prioritize the development of the network by, in part, establishing specific near-term and long-term actions that can be completed to show progress.
- We recommended that HHS identify an office to oversee the development of the network.
- We recommended that HHS identify and document information-sharing challenges and lessons learned from the COVID-19 pandemic.
More from GAO’s Public Health Portfolio
For more information, contact Jennifer R. Franks at (404) 679-1831 or franksj@gao.gov.