Physician Workforce: Caps on Medicare-Funded Graduate Medical Education at Teaching Hospitals
Fast Facts
Before physicians practice medicine independently, they receive on-the-job training as residents in teaching hospitals. These residents are vital providers of health care during their training, and many stay in the geographic area to practice after their training is completed.
Medicare pays these hospitals to offset some of the costs of training physician residents. For most hospitals, Medicare caps the number of residents it will fund per hospital based on how many residents it funded in 1996.
We found that 70% of hospitals trained more residents than Medicare funded—indicating they can train more physicians now than when these caps were set.

Highlights
What GAO Found
Medicare sets caps on both of its types of physician graduate medical education (GME) payments (direct and indirect) to teaching hospitals. Caps on these payments determine the number of physician trainees—known as residents—that each payment type supports. Hospitals can use other sources of funds to train more residents than these caps. Medicare data show that in 2018, 70 percent of hospitals were over one or both caps on Medicare-funded residents, and 20 percent of hospitals were under one or both caps. For both payment types, hospitals funded significantly more slots over the cap than they left unfilled, but Medicare still funded the large majority of resident slots.
Graduate Medical Education (GME) Residents and Slots by Medicare Payment Type and Funding, 2018
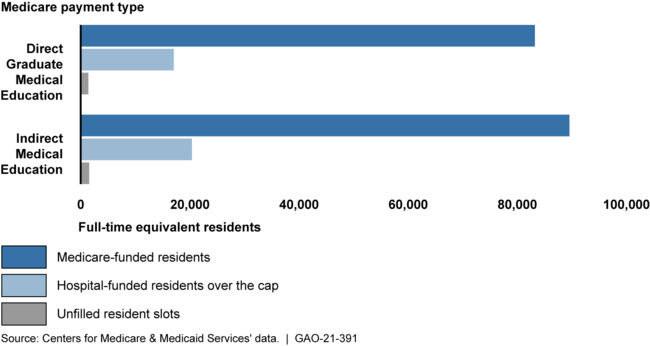
Notes: Medicare's payments for GME are based, in part, on the number of full-time equivalent residents that a hospital trains. Caps reflect the number of residents eligible for the two GME payment types. Direct Graduate Medical Education payments offset direct costs of GME training, such as resident salaries, and Indirect Medical Education payments offset indirect costs of GME training, such as the additional cost of resident supervision.
Medicare gives hospitals starting their first new GME programs 5 years to establish and grow their GME programs before their caps are set. Once set, hospitals' resident caps are generally permanent. GAO asked GME stakeholders about recent proposals to extend this window beyond 5 years. Stakeholders said that extending this time window could result in larger caps and more residents training at some hospitals because the hospitals would have more time to, for example, recruit more faculty and residents or start programs in more complex specialties before caps are set. Some stakeholders representing providers and a researcher suggested targeting the extension to under-resourced hospitals—such as those located in rural areas or areas with health care provider shortages—which often face challenges in quickly recruiting faculty and ensuring a variety of educational experiences for residents. However, they noted that extending the cap-establishment window would not address all challenges that under-resourced hospitals face when starting new GME programs.
Why GAO Did This Study
Studies have shown the United States faces a shortage of physicians, making it increasingly difficult for people to access needed health care. Physicians need GME training before they can practice medicine independently and often practice in the same geographic area as their training.
The vast majority of federal funding for this training—about $15 billion in 2018—supports physician training through the Department of Health and Human Services' Medicare GME payments. Medicare offers payments to teaching hospitals to offset costs of training full-time equivalent residents, up to a capped number of resident slots for each hospital. For most hospitals, caps reflect the number of residents that Medicare funded in 1996; for hospitals starting their first new GME program in 1997 or later, caps were based on the number of Medicare-funded residents trained at the end of a specific time window.
GAO was asked to review Medicare GME funding. This report, among other issues, describes the extent to which hospitals were over or under their Medicare GME caps and stakeholders' views on extending the time window before new caps are established. GAO analyzed 2018 Medicare data (the most recent available at the time of GAO's analysis), reviewed agency documentation, and interviewed eight selected stakeholder groups—including a GME accreditor and groups representing health care providers—identified through past GAO work.
The Department of Health and Human Services provided technical comments on a draft of this report, which GAO incorporated as appropriate.
For more information, contact Michelle Rosenberg at (202) 512-7114 or rosenbergm@gao.gov.
